Nationwide, over 1.2 million people face a lifetime of living with HIV. The disease, which operates by compromising the immune systems of otherwise healthy people, turns commonplace viruses like the flu into potentially life-threatening diseases. However, the real difficulty in fighting HIV is its resilience—it’s very difficult to clear the virus from infected patients. This is because the virus essentially hides in the body, making it less likely to succumb to anti-viral medication.
 What's the best way to wake a sleeping virus? The Zhou and Hurley labs are build- ing viral alarm clocks by boosting Super Elongation Complexes (SECs), kickstarting transcription of HIV genes and coaxing the virus out of its latent state.
What's the best way to wake a sleeping virus? The Zhou and Hurley labs are build- ing viral alarm clocks by boosting Super Elongation Complexes (SECs), kickstarting transcription of HIV genes and coaxing the virus out of its latent state.
Many viruses, such as the flu, enter a cell and then replicate themselves many times before infecting new cells. HIV is different. Instead, the HIV virus inserts itself into the DNA of a cell and stays relatively hidden—sometimes for over 70 years. Scientists have never found a method to eliminate all copies of a virus when they are not actively producing more viruses—also known as the latent state. Current antiviral therapies do not actually kill the viruses. Instead, therapies prevent viruses from infecting healthy cells and multiplying. In other words, these therapies keep HIV dormant, but the virus can spring back to life at any time if a patient stops taking their medication. As a result, patients are never cured and must take medication throughout their lifetimes, which can cost nearly $400,000 per patient, as estimated by the CDC in 2010.
Several recent studies from UC Berkeley have rekindled the hope of curing an HIV infection by luring it out of its latent state, making treatment much more effective. The labs of Qiang Zhou and Jim Hurley, professors in the Department of Molecular and Cellular Biology, have been leading the efforts to investigate this new approach to treating HIV. "One of the conundrums of curing HIV/AIDS is clearing the latent HIV integrated within the genome since the immune system can’t find such cells and destroy them," says Dr. Shiqian Qi, a professor at Sichuan University in China, and formerly a postdoc in the Hurley Lab where he was lead author on a paper published on this work. Their research attempts to understand the biological conditions under which HIV is brought out of its latent state. By tweaking a group of human proteins called Super Elongation Complexes (SECs), researchers may be able to trick the entrenched HIV to stick its head out so therapies have a shot at destroying the virus.
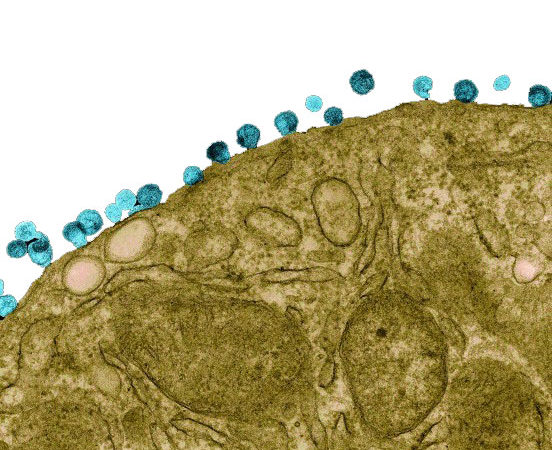 Newly assembled HIV particles (blue) budding from the surface of a T-cell. Image obtained using colorized transmission electron microscopy.
Newly assembled HIV particles (blue) budding from the surface of a T-cell. Image obtained using colorized transmission electron microscopy.
Once HIV inserts itself into a cell's DNA, it relies on the cell’s normal process of gene transcription—the process by which the genes are read so that viral proteins can be produced—to replicate the viral genes. This replication is the first step towards making new HIV viruses, but the process is much slower and more unpredictable than normal cellular genes. Researchers in the Zhou Lab found that SECs play an important role in boosting transcription of HIV genes: a higher concentration of SECs means more genes will be transcribed and more HIV viruses produced. Using a glowing protein derived from jellyfish to report whether HIV genes are transcribed, they found that under normal conditions, the SEC levels are very low in cells, and 99 percent of HIV-infected cells conceal the virus. However, when they artificially boosted the concentration of SEC in the latently infected cells, the hidden HIV was exposed, and the cells efficiently transcribed these HIV genes. In fact, more than 80 percent of latently infected cells showed evidence of active HIV.
Now, Dr. Qi and others in the Hurley and Zhou Labs have been trying to boost SEC levels by making the proteins less likely to be degraded by the cell. By investigating the structure of the purified SEC molecules and examining their assembly in test tubes, the scientists found a small cavity in the center of SEC that makes it unstable. Now, the two labs are trying to develop a drug that can be inserted into this hole to stick the SEC together, increasing its stability and stimulating the transcription of latent HIV.
Though it sounds counterintuitive to promote the creation of more HIV viruses, as Qi explains, "It will help the immune system to eradicate the HIV virus if we can find a way of making the SECs activate the transcription of latent HIV." The approach could be used to coax the latent HIV into making new viruses, which could be coupled with a round of enhanced antiviral therapies that prevent new viruses from infecting healthy cells. Since HIV could no longer hide in the infected cells, the virus could then be recognized by the enhanced immune response and cleared from the body for good.
35 years ago, HIV infection was a speedy death sentence, and treatment was a distant dream; 21 years ago, the advent of antiviral therapies turned it into a treatable, but life-long, chronic disease. Now, with advances in our understanding of HIV and novel methods for treating it, researchers at Berkeley hope to eventually end this devastating pandemic by finding a cure.
Zichong Li is a graduate student in molecular and cell biology studying gene expression. He also likes swimming, biking, and reading.
This article is part of the Spring 2017 issue.