Ask most people and they’ll say that being first is best: you win medals at races, get best dibs on cookies at a reception, avoid getting scooped on research, and ride shotgun in a car. Sometimes, however, being first has both positive and negative consequences, as anyone familiar with the history of HeLa cells can tell you.
HeLa cells have the distinction of being the first immortal cell line cultured by scientists. Unlike a normal population of human cells, which divide about 40 to 50 times before dying away, HeLa cells have the remarkable ability to divide indefinitely. Coming in first secured their status as one of the most popular cell lines used by scientists for research, making them the cornerstone of some of the most significant biological advances. UC Berkeley researchers are also no stranger to HeLa: an estimated 200 labs on campus have used HeLa cells. Today, Berkeley scientists have a wider array of cell lines to choose from, but HeLa’s familiarity and hardy growth continues to make it a popular choice.
In the early 1950’s, however, scientists had yet to meet HeLa. In fact, the original HeLa cells were still attached to a living, breathing human being; a woman who put her family first in every situation, even when battling an unyielding cancer. This cancer would overcome her, but her cancerous cells would continue to grow in laboratories across the world. As the first immortal human cell line, HeLa cells, along with their involuntary donor’s family, had to deal with the growing pains of a society who could develop the technology for cell and tissue culture faster than the ethical rules needed to regulate it.
Both the good and the bad, this is the story of a woman, her legendary cells, and how they have touched the lives of research scientists at UC Berkeley.
A prominent mother figure: paving the way for breakthrough research
For most scientists, Henrietta Lacks represents the mother of all HeLa cells. As the first and, for many years, only cell line able to divide indefinitely out of the body, their popularity among research scientists flourished, and HeLa cells quickly became workhorses in the laboratory. Their first formidable task? To aid in the development of the polio vaccine in 1953. Jonas Salk, a virologist at the National Foundation for Infantile Paralysis, had created a vaccine from inactivated viruses. It seemed promising, but he needed cells—lots of them—to test his vaccine before human trials. HeLa cells were the perfect tool. Not only did they grow vigorously, making it easy to amass the enormous quantity of cells required for the study, but they also become easily infected by the poliomyelitis virus. Within less than a year, the vaccine was ready for human patients.
From there, the list of HeLa’s accomplishments only continued to grow. Known as the mother of virology, cell and tissue culture, and biotechnology, HeLa cells were used to jumpstart research on how viruses act and reprogram cells, as well as to develop standard lab practices for freezing and culturing cells and tissues. Scientists used them to develop cell cloning, in vitro fertilization, and isolation of stem cells, as well as to research AIDS, cancer, and the effects of radiation and toxic substances. HeLa cells have been infected with an array of diseases, from tuberculosis to salmonella, and have helped scientists understand that a normal human cell has 46 chromosomes, thus making genetic disorders easier to diagnose. It is easy to see why many have also named HeLa the mother of modern medicine. HeLa cells were a welcome development for researchers around the world.
 Timeline design: Justine Chia; Henrietta lacks: lacks family; polio: David Goodsell; cloning: NIH; HPV: Ed Uthman; DNA helix: NHGRI; HELA cells: NIH. Click to enlarge.
Timeline design: Justine Chia; Henrietta lacks: lacks family; polio: David Goodsell; cloning: NIH; HPV: Ed Uthman; DNA helix: NHGRI; HELA cells: NIH. Click to enlarge.
A prominent mother figure: taken too soon from her family
For Lawrence, Elsie, Sonny, Deborah, and Zakariyya Lacks, Henrietta was simply known as mom. Described as a strong but caring woman, Henrietta kept her growing family together while her husband, Day, worked at a steel mill. She was no stranger to hard work after growing up with her grandfather on a tobacco farm in Virginia. For the youngest children in the family, however, much of what they know of their mother would come second hand. Henrietta was diagnosed with cervical cancer a mere four and a half months after giving birth to her fifth child, Zakariyya, and would perish from it less than a year later.
Henrietta’s battle with cancer began when, worried about a knot that she felt in her abdomen, she made the 20 mile trip to Johns Hopkins Hospital. At the time, Johns Hopkins was the only option in the area for African Americans seeking medical treatment. A biopsy of her cervix revealed that she had cervical carcinoma, a type of cancer that grows from the epithelial cells that line and protect the cervix. Extensive treatment ensued, which began by inserting tubes of radium into her cervix to reduce the tumor, followed by daily X-ray therapy. Despite the debilitating treatments, Henrietta’s commitment to her family never wavered, and she was able to keep her condition secret from most family members in order to spare them the worry. In turn, she endured much of it alone while Day was at work. Her cancer proved to be too resilient, however, and began to weaken both body and spirit. Tumors overcame nearly all the organs in her abdomen, and relief from the excruciating pain was the only service available at Johns Hopkins. Henrietta passed away on October 4th, 1951.
Her death left a family without its mother.
The birth of HeLa: an exceptional cell line
HeLa as we know it today was born in the lab of George Gey, the director of the Tissue Culture Laboratory at Johns Hopkins Hospital in the 1950s. Gey’s agenda? Cure cancer. His tactic? Develop an immortal human cell line that could be used for research. Fortunately, his position at Johns Hopkins meant he had plenty of tissue samples from which he could try growing human cells in the lab. Unfortunately, most of these cell samples would die within a few generations. That is, until one of them did not: HeLa. Gey obtained HeLa from the surgeon treating Henrietta’s carcinoma, who had been taking cancerous tissue samples from patients for Gey’s research. As with his other samples, Gey named the cell line using the first two letters of the patient’s first and last name. Henrietta Lacks became HeLa.
True to his ultimate goal of curing cancer, Gey was generous with his newly discovered gem, and gave away samples to a few close colleagues working to eradicate cancer. From its beginning in Baltimore, Maryland, HeLa soon traveled the world as scientists far and wide learned of this remarkable immortal cell line.
So what makes HeLa special? As cancer cells, HeLa cells are unlike normal human cells, and there is no better proof of this than to take a look at its chromosomes, or karyotype. Normal human cells have 46 chromosomes, while HeLa has 76 to 80 heavily mutated chromosomes. The origin of this deviation from normalcy stems from the human papilloma virus (HPV), the cause of nearly all cervical cancers. HPV inserts its DNA into a host cell, causing it to begin producing a protein that binds to and inactivates the native p53 protein. p53 is known as the guardian of the genome due to its role in preventing mutations and suppressing tumors. Non-functional p53 protein can therefore have disastrous consequences.
Relative to other cancer cells, however, HeLa cells still grow unusually fast. Gey was amazed to see that within 24 hours of culturing his first HeLa sample, the number of cells had doubled. The source of this abnormal vigor lies in HeLa’s telomerase enzyme. During normal cell division, the string of repetitive DNA at the tips of all chromosomes, known as telomeres, are shortened. This leads to cell aging and ultimately to apoptosis, or cell death. Normal cells have a maximum number of divisions before these telomeres are depleted. HeLa cells, meanwhile, have an overactive telomerase enzyme that rebuilds telomerases after cell division, thus circumventing the aging process and skirting death. This internal fountain of youth is what has allowed HeLa cells to divide indefinitely, making them now older than Henrietta was when she died.
The birth of HeLa: at the expense of proper consent
For decades, Henrietta’s side of the story has been largely ignored, but thanks to Rebecca Skloot’s novel, The Immortal Life of Henrietta Lacks, she finally has a voice. When Henrietta stepped into the public ward of Johns Hopkins on January 29th, 1951, she could have had no knowledge of what was to ensue. She hoped that her radium treatments would cure her of cervical carcinoma. She hoped that she would still be capable of having children. She hoped to see her family thrive and grow. Unfortunately, she was let down on many counts; Henrietta’s cancer proved too powerful for the doctors at Johns Hopkins to treat, despite their best efforts.
No effort, however, was made to treat Henrietta herself as a woman capable of making her own medical decisions. Without question, Henrietta would have opted out of treatment had she been informed that it would leave her infertile, a fact that she only discovered once it was too late. She also never discovered that her surgeon had taken tissue samples for Gey’s research. Would she have consented? Would she have appreciated Gey sending her cells to his colleagues? What about having her cells commercialized and sold for profit, as they are commonly done today? Would she mind that strangers would profit from her cells, selling them to researchers making important medical advances, while her own family is unable to pay for health care?
It’s too late for Henrietta to answer these questions, but her story has forced scientists and doctors to make sure that such questions are addressed by patients and research participants. Since 1991, scientists and doctors have been governed by the Common Rule, which requires them to inform people when they are participating in research, and that their participation be completely voluntary. Patients must sign consent forms which clearly state what the research is, how long it will last, what the potential risks are, if there is any compensation, and more. Unfortunately, the Common Rule did not come soon enough to protect Henrietta’s family. After HeLa cells exploded on the scene and became associated with many significant scientific advances, people became curious about the woman behind the cells. Along with consent, anonymity and privacy were not issues that had been properly addressed in the medical arena, and Henrietta’s identity was soon revealed. Having her name so closely related to HeLa probably did not help.
This is how, 22 years after her death, Henrietta’s children learned that pieces of their mother were still alive and thriving. Scientists came knocking, asking for blood samples to supply the genetic information needed to better understand HeLa. Again, no consent was obtained, and with a limited background in biology, the family misunderstood the purpose of these samples; they thought they were being tested for cancer. Marginalized by the media and the medical community, it would take decades for them to uncover the true story of what happened to their mother and to gain an understanding of what HeLa means to the world today.
Life in the lab as a hearty membrane source
When Pengcheng Zhang steps into his lab in Li Ka Shing Center to start another day, he is often met by HeLa. Zhang is a fifth year molecular and cell biology PhD student working in the lab of Professor Randy Schekman. The Schekman lab focuses on understanding how proteins produced in a cell are shuttled out via the secretory pathway, an intricate assembly of membranes and proteins. Schekman’s goal is to decipher this pathway by pinpointing the proteins and biomolecules that make it run, and determining just how they do it. So far, he has been successful in yeast.
 Credit: Design: Justine Chia; Globe: NASA Data source: Rebecca Skloot Click to enlarge.
Credit: Design: Justine Chia; Globe: NASA Data source: Rebecca Skloot Click to enlarge.
“[Schekman] started out in yeast because it’s much less complex than tissues and organs,” explains Zhang. “After about 20 years of work they came up with this protein complex called COPII, which is required for the first step into this secretory pathway.”
COPII (coatomer protein complex II) is a set of five proteins that work together to create vesicles, or sacs, that bud from protein-producing subunits in the cell, known as the endoplasmic reticulum. These vesicles are then transported to other membranes in the cell for unloading, including export through the outer membrane. The Schekman lab was able to recreate the process in test tubes with only the cargo, purified yeast membranes, and COPII, thus identifying the key components required for the secretory pathway. “This is a very central concept in biochemistry: that we can reconstitute biological processes in the test tube,” says Zhang. “We look at biological processes as a series of chemical reactions.”
Although cells are composed of a vast amount of material, if the proper proteins or biomolecules required for a given cellular reaction are identified and isolated, that same reaction can be carried out in a cell-free system. This is how the Schekman lab was able to identify and isolate the COPII complex of yeast. More recently, however, they have set their sights on understanding the secretory pathway in higher order organisms such as mammals. “We know for a fact that in mammals COPII does the same thing,” explains Zhang. “But the thing is, from yeast to humans the number of proteins that go through the secretory pathway expands.”
For some of these larger, more complex proteins, the Schekman lab has found that COPII alone is insufficient in their test tube “cell”. Understanding the modifications, such as additional proteins, that are required for mammalian cells is now the goal. Zhang, for instance, is trying to understand the necessary components for shuttling transforming growth factor alpha (TGF-α), a protein that is involved in the development of epithelial tissue such as skin or the lining of the cervix. This is where HeLa comes in. “HeLa cells are the major membrane source for my biochemical reactions,” says Zhang. “They are desirable in our case because it’s a human cell line and it grows relatively fast.”
Faster growth means more membranes for Zhang’s experiments. Zhang also uses another mammalian cell line derived from rat liver cells to harvest its cytosol, which is the cellular fluid containing all the proteins and biomolecules of the cell. Zhang transfects, or introduces, additional TGF-α cargo into these liver cells in order to yield better signals. By combining purified COPII, HeLa’s cell membranes, where the secretory mechanism occurs, and the harvested cytosol containing the TGF-α cargo and Zhang’s mystery proteins, Zhang has all that he needs to recreate the secretory pathway in vitro. The trick, however, is figuring out which protein or proteins in the cytosol are doing the work.
“We fractionate the cytosol, separate the protein content, and analyze where the activity goes,” explains Zhang. When one of the fractions successfully reproduces the secretory pathway, Zhang knows that it contains his desired protein. Unfortunately, it’s usually not the only protein present. “[The fractions are] not pure enough that we can assign the function to a particular protein or couple of proteins with confidence. That’s why we need many fractionation steps to get down to a pure enough fraction to have confidence to say that we think these things are responsible for this secretory function.”
So far, the protein of interest remains a mystery. Once identified, however, the Schekman lab can determine if changes or mutations in the protein are linked to any human diseases, with the ultimate goal being treatment of such a disease.
Zhang is not the only graduate student at Berkeley taking advantage of HeLa’s utility in the lab. Ann Fischer, who has been running the Tissue Culture Facility in Barker Hall since 1989, supplies HeLa cells for many of the labs who use them today. She is no stranger to HeLa: Fischer has been working in tissue culture facilities, first at UCSF, then at UCLA, and finally here at UC Berkeley, since 1971.
Fischer says the use of HeLa cells by UC Berkeley researchers has gone through various phases during her time here. Initially, she would grow hundreds of liters of HeLa cells for researchers in the biochemistry department to extract large quantities of a given protein of interest.
“That was the heyday of just biochemistry: using cells to get proteins out,” explains Fischer. “People [later] started using cells for overexpression.” Overexpression involves inserting a gene of interest into the DNA of HeLa cells and stimulating the cells to express it, thus enabling researchers to obtain larger quantities of protein with fewer cells. Today, overexpression is still a popular application of HeLa cells, but the utility of HeLa has expanded. Zhang, for instance, uses HeLa to harvest its membranes, while others take advantage of HeLa’s large size for imaging. In the end, HeLa’s vigor is what makes it so popular.
“It’s because they grow so well,” explains Fischer. “That’s the reason people use HeLa cells.”
Life in the lab: as a hearty contaminant
When Professor Gertrude Buehring steps into her lab in Koshland Hall, she is never met by HeLa cells. In fact, she makes a point of it. “We never grow them,” she says. “I wouldn’t want to take that risk, actually.”
Buehring, a professor of virology in the School of Public Health, has a reason to be wary of HeLa. Both her PhD and postdoc careers were spent working at UC Berkeley’s Cell Culture Laboratory housed in the Naval Biosciences Laboratory in Oakland, a cell repository funded by the federal government that characterized and maintained cell lines for research scientists. She happened to be working there at a time when Dr. Walter Nelson-Rees, the co-director, was working hard to expose HeLa’s misdeeds. The vigorous cell’s crime? The contamination of other, less hardy cell lines.
Nelson-Rees was not the first to suspect contamination by HeLa cells. In the 1960s, Dr. Stanley Gartler, a research geneticist, released the initial “HeLa bomb”. Gartler had discovered that the 18 different cell lines he had collected for his research all turned out to be genetically identical, with genes only present in people of African descent. HeLa was a suspect, but many scientists refused to accept the implications of his discovery, and chose instead to ignore it. Ten years later, Nelson-Rees picked up where Gartler left off, and discovered several HeLa specific chromosomal markers that could be used to test the identity of cell lines.
“Since this repository had so many cell lines, [Nelson-Rees] was going through all of them and examining them for these markers,” recalls Buehring. “While he was there he came up with 40, which was more than one expected.”
In that instant, any tissue-specific research that used the cell lines identified as HeLa contaminants was suddenly invalid. How can research on breast cancer cells be taken seriously when the cells used were actually cervical cancer cells all along? It has been estimated that over 500 research papers and more than 20 million dollars of funding have been wasted. The problem stems from the adolescent days of cell culture.
“After Dr. Gey established the HeLa line, everybody was so excited and thought they could establish a human cell line, too,” Buehring explains. Unfortunately, most of these labs did not have the knowledge or equipment to properly culture cells. What they did have was plenty of HeLa cells around, and due to HeLa’s hardiness, a single cell could outgrow and overtake all normal human cells in a culture. “Suddenly everybody was able to establish a human cell line,” jokes Buehring. It turned out that many of them were just HeLa.
Even years after being exposed for what they really were, HeLa contaminants continued to be sold by the American Type Culture Collection (ATCC), one of the largest international cell line repositories, and scientists continued to request the cells they had become so familiar with. In fact, many scientists were hostile towards Nelson-Rees, and unable to accept the implications of his work. Over time, however, the ATCC refused to sell HeLa contaminants. This doesn’t mean, however, that they are no longer used in labs today. Since her days working at the Naval Science Laboratory, Buehring kept HeLa in the back of her mind, and was curious about the extent to which HeLa contaminants were still used, as well as how aware researchers were about HeLa’s potency.
“I couldn’t find any research papers where people actually looked at that,” she says. So in 2004 she decided to look into it herself. With the help of an undergraduate student, Professor Buehring conducted a survey of researchers known to culture cells, and asked what kinds of cell lines they worked with, whether it was for tissue-specific work or not, and if they ever tested the identities of their cell lines. The results surprised her.
“There were so many people who used HeLa cells in their laboratory, and only about 50% did any kind of check to see if there was contamination,” she says. Not only that, but about 60% of respondents had acquired at least one cell line from another laboratory rather than from a repository like the ATCC.
“Often times people will think they’re getting a good cell line from a colleague down the hall, but they don’t know it’s already been contaminated,” she explains. “If it isn’t checked, you never know that.” Buehring herself rarely gets cells from other labs, but if she does, she makes sure to check their identity before trusting them.
The survey also revealed that about 10% of respondents still used HeLa contaminants, 30% of which used them for tissue-specific purposes. The original “HeLa bomb” of the 1960s and 70s had lingering effects, it appeared.
The truth is, however, that many researchers today don’t see HeLa as a contamination threat anymore. “Back when cell cultures started, they were using glass. It was so easy to contaminate,” says Fischer. The use of disposables today helps eliminate some of the threat. “Nowadays, I don’t worry about that at all.”
Like Buehring, Fischer also insists on getting cells from reputable sources like the ATCC; otherwise, she suggests verifying their identity. Going back to frozen stocks of cells every week or two is another method of avoiding contamination. Zhang says that he, too, is not concerned. “If it gets contaminated with a different cell line it’s very recognizable because looking under the microscope every cell line has a very distinct shape,” he explains. HeLa cells, for instance, are often very large and triangular.
Not only have cell culturing methods improved, but HeLa’s days as the easiest and fastest growing cell line are over. New cell lines have emerged that work just as well, if not better, for certain applications. Insect cells, for instance, can also be used to overexpress proteins, but can be grown in larger quantities. This makes them ideal little protein factories for when researchers need large quantities of a given protein for study. “People don’t use HeLa cells as much because they’re harder to grow than insect cells,” says Fischer. “Believe it or not! Harder to grow!”
Bacteria cells are actually the easiest cell type to grow, but may not be capable of making some of the more complicated human proteins that often require more intricate modifications before they become fully functional. Yeast cells, which have a more advanced protein assembly system, are the next line of attack, followed by insect cells. Only if these three cell types are unable to produce the human protein of interest do researchers consider human cells such as HeLa.
There are other reasons that HeLa cells are finding themselves at the bottom of the list: as a cancer cell, its DNA is a major liability. “[HeLa cells] have the strangest karyotype,” says Fischer. “They have 3 copies of this, and 2 copies of this, and 5 copies of that. They’re not normal.”
 The karyotype of a HeLa cell is very different from the karyotype of a normal human, with extra copies of some chromosomes and missing copies of others. credit: Duesberg lab, UC Berkeley
The karyotype of a HeLa cell is very different from the karyotype of a normal human, with extra copies of some chromosomes and missing copies of others. credit: Duesberg lab, UC Berkeley
Many researchers today choose to work with cells that more closely resemble normal human cells, thus taking their in vitro systems one step closer to mimicking how a real human functions. IMR-90 cells are one such example. Cultivated from the lungs of a human fetus in the Netherlands, IMR-90s have a normal karyotype with 46 chromosomes. Of course, there are drawbacks to working with “mortal” cells.
“They only go up 60 populations and then they [die],” says Fischer. “We have to thaw those every three weeks.” Not only that, but as the cell line becomes older and older, they show signs of aging and may not be ideal for research anymore. Luckily, Zhang doesn’t have to worry about trying to work with more normal, but finicky, cell lines.
“Since we’re looking at such a fundamental process in the cell, we think that although HeLa cells are very different from normal human cells, the basic processes that keep the cell alive should essentially be unaltered,” reasons Zhang.
Buehring agrees that there is an important distinction between using HeLa to obtain basic cellular material versus using HeLa as a whole cell and expecting all of its cellular processes to be the same. As a “bag to hold the biomolecules of study,” however, they work just fine. For other purposes, HeLa may not be top dog anymore.
A wealth of information: making research faster and easier
Like a celebrity, the more scientists learn and work with HeLa, the more popular it becomes. It began in the early days of cell culture, when HeLa’s vigor and human origin made it unique. Today, scientists take comfort in HeLa because of its familiarity.
“It’s well-characterized because so many labs have been working on it,” explains Zhang. “There are many tools that work with HeLa cells that don’t necessarily work well with obscure cell lines.”
This is because many of these tools or techniques were originally developed using HeLa cells, and are thus optimized for them. One example, gene knockdowns, can be used to stop HeLa from expressing a specific protein, thus helping Zhang determine if and how it affects the secretory pathway. HeLa also has good transfection efficiency, ensuring that when Zhang transfects his HeLa cells with a protein, a higher percentage of the population will have his protein of interest.
Not only can HeLa do a lot, we also know a lot about it. As a human cell line, the human genome database becomes an important source of genetic information. Zhang, for instance, uses the database to design his knockdowns and target a specific gene of interest. Though not crucial, HeLa’s specific genome would make things even easier. Luckily, this is now a possibility. Since August of 2013, researchers can submit proposals to gain access to the HeLa genome on the National Institute of Health’s (NIH) database.
“You would know which genes are expressed instead of empirically testing it, which can take a week,” says Zhang. Access to the NIH database would let him see what genes are expressed and to what degree, therefore making it easier to design effective knockdowns.
Simply put, HeLa cells are just plain simple.
A wealth of information: crossing the boundaries of privacy
As HeLa’s popularity in the lab grew and the list of medical discoveries reached the ears of non-scientists, public interest sprouted. Articles began to surface that speculated on the identity of this mystery woman. Credit was given to Helen Lane or Helen Larson, until eventually Henrietta’s true identity was revealed.
Researchers, members of the media, and con artists soon hounded the family, all hungry to use them for their genetic information, family history, or as pawns for a fraudulent money-making lawsuit against Johns Hopkins, respectively. No one, however, provided the family with any information in return, and they were often left in the dark about their mother’s final months, the origin of HeLa, and the implications of HeLa in research. The infamous cells became a burden.
This kind of disclosure about a human cell line would be unthinkable today, and rightly so. “Nowadays, if you take their cells, you wouldn’t call them by that patient’s name because of confidentiality,” says Fischer. “What if you found a genetic abnormality that could be traced back to the family?”
Which is, in fact, a very real question posed by members of the Lacks family. In March of 2013, HeLa’s complete genome was published without the family’s knowledge. Researchers like Zhang sit on both sides of the fence on the issue. “It would be helpful to get some genomic information that would be specific to HeLa cells,” he begins, “but there’s this privacy issue, an ethical issue.”
The genome was removed after the family voiced its concerns. A few short months later, however, a compromise was reached, known as the HeLa Genome Data Use Agreement. Researchers can obtain controlled access to the genome after submitting a proposal, and any data obtained from the genome must be openly shared on the NIH database. Access to the genome will be tightly regulated by a committee of six, two of whom are members of the Lacks family.
It may not have been a simple journey, but the family is in the dark no more.
Over the years the family has come to learn about the use and importance of HeLa cells, and the research and medical communities have, in turn, learned to respect them. Credit, in large part, must be given to Rebecca Skloot, whose book, The Immortal Life of Henrietta Lacks, was the first to focus on the story of Henrietta and her family rather than HeLa. Skloot took a different, more constructive, approach than the scientists and members of the media who came before her. She chose to work with the family rather than use them, and helped them understand all parts of their mother: from life to death to HeLa. In turn, scientists can now learn about the history of the cells they have become so familiar with in the lab, and understand their significance outside of the lab.
“The wealth of information that we’ve learned from her cells is just so overwhelming,” says Zhang. Not only has this information resulted in valuable medical advances, research papers, and PhD theses, but also in crucial laws and policies governing the use of cells and tissues, and a greater awareness of cell line contamination. It may be that with good comes bad, but the key is converting the mistakes of the past into something constructive for the future. Zhang would argue that acknowledging those who deserve the credit is also important: “I think we should all be grateful to her.”
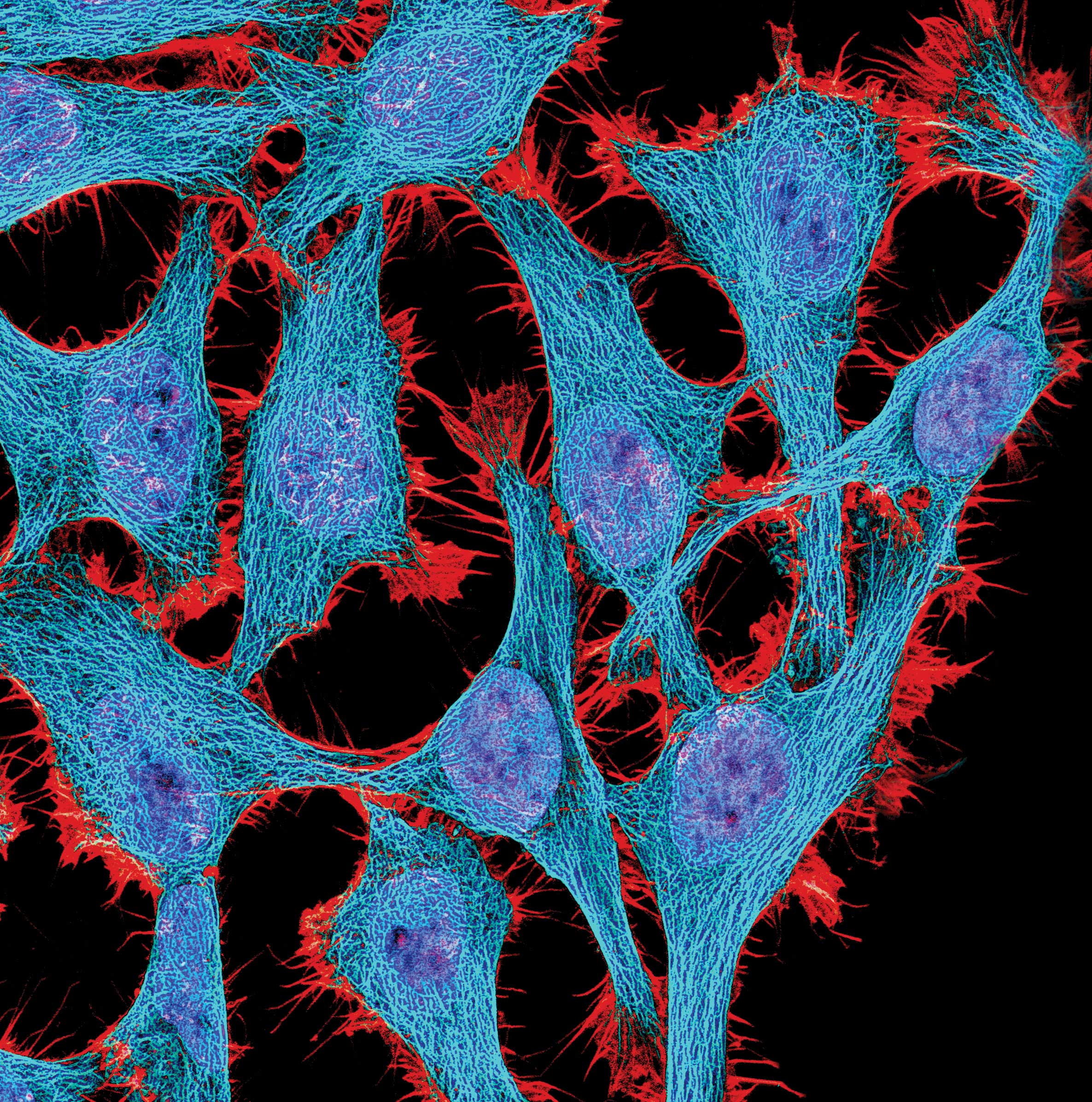
Featured image credit: NIH
This article is part of the Spring 2014 issue.



